August 9, 2019
Nanoparticles: tiny molecules show big promise

Scientists at MIT have devised new methods of delivering medication to hard-to-treat brain tumors like glioblastoma that use a kind of tiny molecule called “nanoparticles.” The MIT scientists had a pair of drugs that they believed might prove effective, but to make them work, they needed to find a way to cross the blood-brain barrier. So they turned to nanoparticles.
According to the National Cancer Institute, this physical barrier in the central nervous system protects delicate neurological tissue from harmful agents. Yet this presents a challenge: if it can stop things from reaching brain tissue, then it can also prevent chemotherapy treatments from reaching the brain tumor cells that they’re designed to attack. Certain nanoparticles, like the ones developed by MIT’s researchers, can not only pass across the blood-brain barrier, they can in effect “escort” a drug into regions that it would be unable to reach on its own.
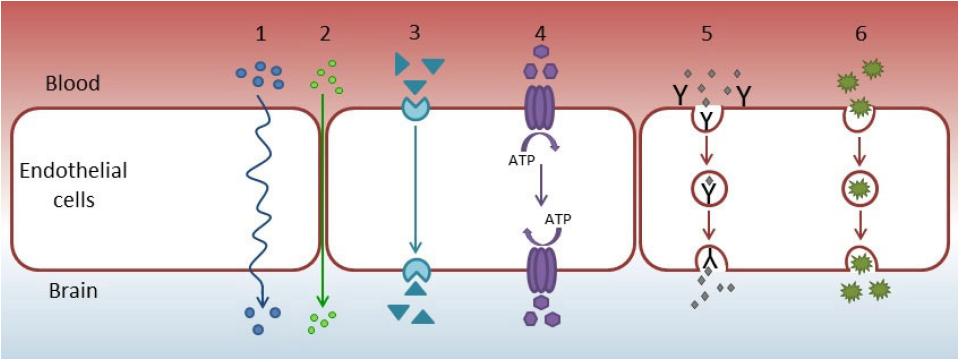
Nano- is a term used by scientists to mean extremely small. In this case, it refers to molecules that are between one hundred and ten thousand times smaller than a typical human cell. Because of their small size, nanoparticles can easily pass into many types of cells and pass through blood vessels as they circulate through the body. This has a number of useful applications in medicine and in particular brain tumor treatment.
The nanoparticle developed by the MIT scientists consists of 4 main elements. First, it has a spherical shell for structure. Second, inside the shell is a drug – in this case the widely used chemo agent temozolamide (TMZ). Next, there is a second drug on the outside of the shell – a substance known as a bromodomain inhibitor that prevents tumors from repairing themselves after they’ve been attacked by TMZ. Last, the whole thing is coated with an enzyme called transferrin that acts as a key to allow passage through the blood-brain barrier.
In mouse trials, the researchers found the coated nanoparticle far more effective at shrinking tumor cells than TMZ alone.

This kind of one-two punch, where the first drug attacks the tumor and the second one prevents its repair, is a common chemotherapy strategy in the rest of the body. Yet it has historically been difficult in brain tumors because of the blood-brain barrier. Even without the development of new anti-tumor agents, nanoparticles seem to promise a way of using the drugs we already have more effectively.
Chemotherapy delivery isn’t the only useful application of nanoparticles. They’re already widely used to improve visibility of brain tumors during surgery. Certain nanoparticles can be injected into the brain that cause tumors to more clearly “light up” under an MRI. This means a neurosurgeon can see what is tumor and what is healthy, and achieve a more complete resection (aka removal) of tumor.
Another study conducted by Massachusetts General Hospital found that combining nanoparticle drug carriers with bursts of low dose radiation, they could achieve five times better drug uptake in mouse models of glioblastoma.