March 20, 2024
Potential Side Effects of Treatment and Tips on Management
How chemotherapy drugs work to treat brain cancer
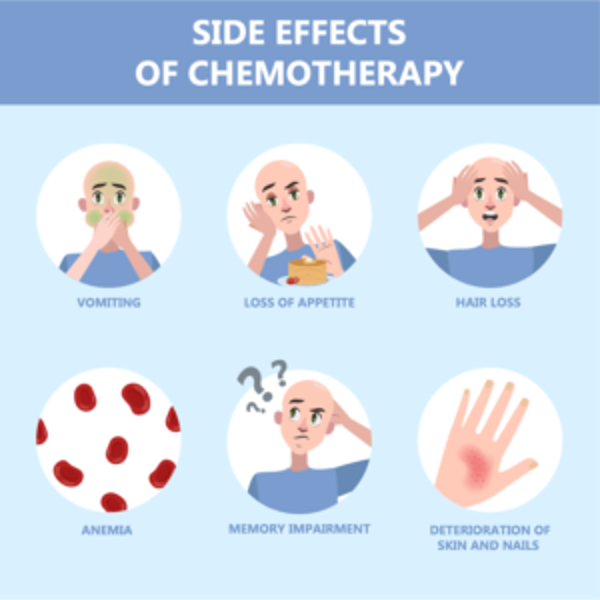
Classical chemotherapy medications indiscriminately affect any cells growing faster than the average cell in our bodies. That defines cancer, but also can include hair/skin/nails, the lining of the gastrointestinal tract (mouth, stomach and intestines) and the bone marrow (where our blood cells are made). That is why these drugs can cause hair loss, nausea, and decreased blood counts.
Targeted therapies may block specific growth factors in your tumor. Immunotherapies work to excite your own immune cells to attack the tumor cells. Even within different drug categories, each drug is unique, however, and can cause different side effects.
How common are side effects from medications used to treat brain cancer?
Side effects are extremely common among patients receiving chemotherapy of any kind, in fact one study found that 86% of patients experienced at least one side effect during their chemotherapy treatment. However, while all chemotherapy treatments have common side effects, patients shouldn’t expect to experience all of the common side effects associated with a specific medication. Just like each brain tumor is unique, so is the experience of each patient.
One thing that almost all patients with brain cancer share is experiencing the side effects of the treatment for their tumor. Unwanted or problematic effects of medication that are beyond the intended scope of their use are all side effects. They might be minor, or they could be extremely debilitating, but side effects are usually consistent, and once you’re used to the medication, they can even be fairly predictable. Knowing what to look for can help you and your treatment team manage side effects as they occur.
Are side effects for chemotherapy treatment of brain cancer treatable or reversible?
Yes. Your treatment team can help you with additional medications to ease your experience of any side effects that you may be experiencing during chemotherapy. Some people find that keeping a journal to track your medication and any reactions helps to track side effects, making it easier to report any issues to your doctor. Your doctor may also refer you to a palliative care team to help with managing side
effects.
Additionally, almost all side effects are reversible, meaning they should disappear after a chemo treatment cycle is complete. Some may fade quickly, in a few days, while others may take a few weeks to completely resolve.
Different Medication Types and their common side effects
The side effects we’ve listed below are understood to be “common” among patients, meaning that over 30% of people who use the medication report experiencing one or more of the symptoms.
Avastin (Bevacizumab)
- Generalized Weakness
- Pain
- Abdominal pain
- Nausea & vomiting
- Poor appetite
- Constipation
- Upper respiratory infection
- Low white blood cell count (This can put you at increased risk for infection)
- Proteinuria (kidney problems)
- Nose bleed
- Diarrhea
- Hair loss
- Mouth sores
- Headache
Carboplatin
- Low blood counts (including red blood cells, white blood cells and platelets)
- Nausea and vomiting usually occurring within 24 hours of treatment
- Taste changes
- Hair loss
- Weakness
- Blood test abnormalities: Abnormal magnesium level
Cisplatin
- Nausea and vomiting. Nausea may last up to 1 week after therapy. Anti-nausea medication is given before the infusion, and a prescription is also given for use after.
- Low blood counts. Your white and red blood cells and platelets may temporarily decrease. This can put you at increased risk for infection, anemia, and/or bleeding.
- Kidney toxicity. Effects on kidney function are dose related, observed 10-20 days after therapy, and are generally reversible.
- Ototoxicity hearing loss, ringing in the ears.
- Blood test abnormalities (low magnesium, low calcium, low potassium)
Irinotecan
- Diarrhea; two types early and late forms.
- Early diarrhea: Occurring within 24 hours of receiving drug, accompanied by symptoms runny nose, increased salivation, watery eyes, sweating, flushing, abdominal cramping. (This can occur while the drug is being administered. If so, alert your healthcare professional promptly. Medication can be given to stop and/or lessen this early side effect).
- Late diarrhea: Occurring greater than 24 hours of receiving drug, usually peaks at about 11 days after treatment. Because of concerns of dehydration and electrolyte imbalances with diarrhea it is important to be in contact with health care professionals for monitoring, and for medication and diet modifications advice.
- Nausea and vomiting.
- Weakness.
- Low white blood cell count. (This can put you at increased risk for infection).
- Low red blood cell count (anemia).
- Hair loss
- Poor appetite
- Fever
- Weight loss
Lomustine
- Low blood counts (bone marrow suppression). Your white and red blood cells and platelets may temporarily decrease. This can put you at increased risk for infection, anemia and/or bleeding.
- Nausea and vomiting. Usually within 3-6 hours of taking medication. Taking dose at bedtime, with an anti-nausea medication, significantly reduces the incidence and severity of this side effect.
Temodar (Temozolomide)
- Nausea and vomiting
- Constipation
- Headache
- Fatigue
Tips from Cancer patients who’ve been there
1. Get some rest
Fatigue is the most common side effect experienced by cancer patients, especially those undergoing chemotherapy. So, get plenty of rest and avoid pushing yourself too hard, even if you feel good. Be patient with yourself and others since it may take some time to get back to your regular energy levels. And, remember that it’s OK to ask for help so that you can take it easy.
2. Stay hydrated
Diarrhea, vomiting and other chemotherapy side effects can cause you to become dehydrated. Not only can this cause you to have low energy, but it can also cause other health issues. So, be sure to drink plenty of water during your treatment. Decaffeinated tea, juices and milk can also help. If you’re having trouble consuming enough liquids or staying hydrated, talk to your care team.
3. Eat when you can
Chemotherapy can cause nausea and appetite loss, so it’s important to eat when you can to avoid becoming malnourished. Keep in mind that many foods may taste different as you go through treatment. For some patients, food may have a metallic aftertaste during and after chemotherapy.
4. Create a sense of normalcy in your routine
Stick to your normal routine as much as possible. That could be something as small as getting dressed up every day, or having a meal with your family. These rituals can help take your mind off cancer.
5. Look to your support and care teams to have your back through treatment
Going through chemotherapy is tough, so look to your family, friends and your care team for support. The doctors and nurses will do everything they can to make you comfortable. But it’s important that you ask questions and voice concerns, so they can help.
6. Keep things around that bring you comfort
Bring your favorite blanket, a yummy snack, your best friend, a good book or whatever brings you the most comfort and keeps you busy while you wait.
7. Stay ahead of your nausea
Many patients experience nausea during and after chemotherapy. So, get your nausea prescriptions filled before you start chemotherapy, and take them before treatments so they kick in before the nausea does. If your nausea medications don’t work, ask your doctor to try a different prescription. It might take a few tries to find the one that works best for you.
Sitting outside and getting some fresh air may also provide a little nausea relief. Popsicles, mints and gum may, too. Sniffing alcohol pads or even alcohol based hand sanitizer is another trick.
8. Stay positive
Sometimes our fears are worse than the reality, and each day of treatment can surprise you. Seek out the positives in your day – small and insignificant as they might seem – to keep your spirits lifted.
9. Prepare for possible hair loss
Most cancer patients who undergo chemotherapy experience hair loss, usually starting around seven to 21 days after the first treatment. For some, hair falls out gradually, while others wake up with big clumps on their pillow. But whether you lose your hair depends on the type and dosage of chemotherapy you’re receiving. Talk to your doctor about what to expect before starting treatment, then make plans for what you’ll do if and when you lose your hair. You might consider cutting your hair short or shaving your head once you start losing your hair, for instance, or decide to try out scarves, wigs, turbans or hats.
10. Remember that everyone’s experiences with chemotherapy is different
You’ll get lots of good advice, your experience with chemotherapy won’t necessarily be the same as that of another patient. Some people may want to stay in bed for days after chemotherapy, while others can go about their normal routine within a few days. And some patients lose their hair quickly, while others keep their hair longer – or don’t lose it at all.
So, go easy on yourself, pay attention to your side effects and share your questions and concerns with your care team.
Radiation Therapy Side Effects
Radiation not only kills or slows the growth of cancer cells, it can also affect nearby healthy cells. Damage to healthy cells can cause side effects.
Many people who get radiation therapy have fatigue. Fatigue is feeling exhausted and worn out. It can happen all at once or come on slowly. People feel fatigue in different ways and you may feel more or less fatigue than someone else who is getting the same amount of radiation therapy to the same part of the body
| Part of the body being treated | Possible side effects |
| Brain |
|
Why brain tumor treatment has you feeling more tired than you’ve ever felt, and steps you can take
Fatigue is the most common side effect of brain tumor treatment. All the major forms of cancer treatment, including chemotherapy, radiation, and even surgery recovery can cause fatigue.
Fatigue is more than simple tiredness. It is a widely-recognized medical condition, marked by extreme lack of energy, which can cause inability to function in daily life. It may be acute – lasting a short time in connection with a direct cause, or chronic — becoming a long-term fact of life for someone affected.
According to the NIH, fatigue related to cancer is different than what healthy people feel. Healthy people’s fatigue is generally relieved by sleep and rest. But for someone with a brain tumor, especially if they’re undergoing treatment, it is normal to experience some fatigue all the time, and for it to become very serious from a light amount of activity.
Even compared with other cancers, brain tumors can lead to especially severe cases of fatigue. Dr. David Cachia of the Medical University of South Carolina told Cancer Network that one study found 96% of patients with high-grade gliomas to experience moderate to severe fatigue. It’s not limited to the worst brain tumors either. Another study found that 39% of patients with lower-grade gliomas, interviewed more than 3 years after finishing treatment, still reported bouts of severe fatigue.

Dr. David Cachia of the Medical University of South Carolina says that patients in active treatment and with other symptoms are more likely to experience deep, lasting fatigue.
Dr. Cachia pointed out a few other contributing factors for fatigue. Patients in active treatment are more than twice as likely to experience fatigue. Patients with many other symptoms, such as pain, distress, or weakness, were more likely to experience fatigue. This is called symptom clustering. And women are 2.5 times more likely than men to report severe fatigue.
If you’re experiencing extreme or worsening fatigue, that’s something to speak with your doctor about. You may be experiencing side effects from medication or it may be a sign of something that warrants medical attention.
Additionally, taking steps around an overall positive and healthy lifestyle can make a difference:
- Eat a healthy and balanced diet.
- Take time to relax, and save your energy for when you need it. It’s OK to do less than you’re accustomed to.
- Practice good sleep habits, such as turning off the tv and limiting screens or highly stimulating activities close to bedtime.
- Stretch and do some light exercise if you’re able to.
- Get a massage. There’s actual research that massage helps with cancer-related fatigue and overall quality of life.
Resources