May 17, 2020
Research Roundup: AI to read brain scans, progress in immune treatments
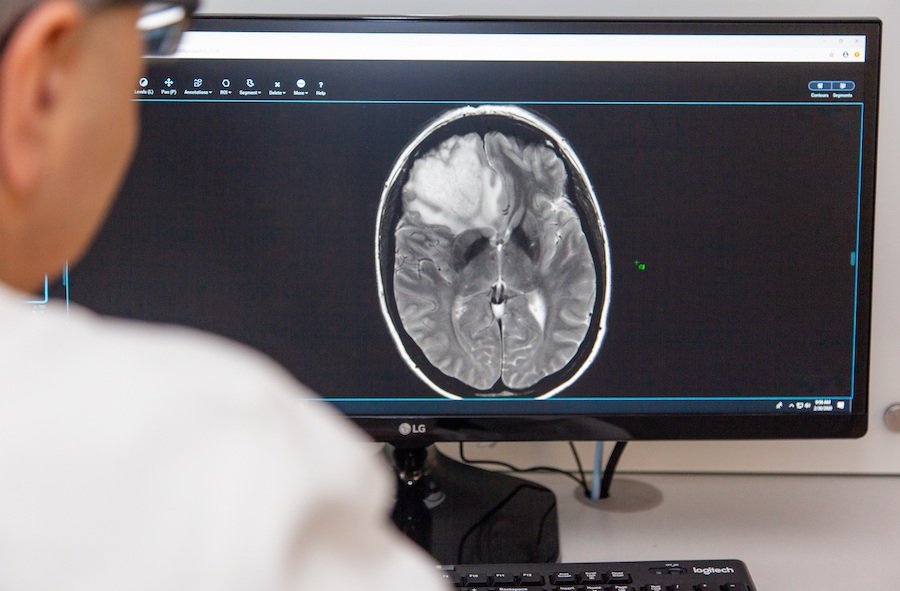
UT Southwestern: AI may help brain cancer patients avoid biopsy
Brain tumors vary a lot, and those variances shape what kind of treatment is most appropriate. A typical journey for a person with a brain tumor goes like this: an MRI produces a preliminary brain tumor diagnosis, followed by surgery to remove the tumor, and then a biopsy—that is, a detailed chemical analysis—gives doctors a clear understanding of what key traits and mutations a tumor has. Only then can the rest of the treatment plan come together.
But researchers at UT Southwestern’s O’Donnell Brain Institute have developed a new AI that can determine the key mutations in a brain tumor from scans alone—no surgery necessary. They’re using a “deep learning” AI model, which is the same technique your phone’s photos app uses to identify faces. The technique classifies the mutation status of a brain tumor from 3D scans with over 97% accuracy. The researchers are planning some additional experiments but they hope that it will lead to more patients with gliomas able to be treated without resorting to surgery.

UF brain tumor researcher embarks on first-in-human clinical trial of novel immunotherapy vaccine
A pediatric oncologist at the University of Florida will launch the first in-human trial of a brain tumor immunotherapy treatment this summer. All immunotherapy techniques for cancer are based on the principle of teaching the immune system to recognize cancer cells as foreign invaders.
Dr. Elias Sayour has developed a technique that extracts genetic material from a patient’s own tumor, encases it in a fat-like nanoparticle, and injects the particles into patients. To the immune system, these particles look like a dangerous virus, and this triggers an immediate strike, not just on the injected particles, but on the similar-looking tumor cells.
UCalgary study finds a common vitamin may help our immune system battle a deadly brain tumour
Researchers at the Cumming School of Medicine at the University of Calgary recently published a new study that showed that combining Niacin, aka vitamin B3, with chemotherapy, helps the immune system attack glioblastoma cells, which can dramatically slow the advance of the disease.
One reason glioblastoma is so deadly is that it often hijacks the immune system, causing it to help the cancer instead of destroying it. The researchers found that this common compound can help reverse that and give drugs and the immune system the leg up it needs.
However, the lead researcher of the study, Dr. Wee Yong, cautioned that just because the findings involve a widely available compound, people shouldn’t try and dose themselves. “It’s extremely important to follow strict protocols and conduct a clinical trial first, even though this treatment involves two well-known, existing therapies. It’s important people don’t rush out and try adding niacin on their own, as we need to confirm dosage, delivery and length of time for optimum clinical results,” Yong told UCalgary News.
Therapy Harnesses Immune System to Slow Progression of DIPG Brain Tumors
Diffuse intrinsic pontine glioma, or DIPG, is one of the most common and most deadly forms of pediatric brain tumors, and it is usually inoperable because it attacks the brain stem.
Researchers at the University of Michigan have found positive results in mouse models using a gene therapy that stimulates the immune system. Normally, DIPG tumors suppress immune system activity in their surrounding tumor microenvironment. But the researchers introduced a gene called TK/Flt3L, which encourages immune activity in the region. They found that introducing this gene increases immune activity around the tumor without causing adverse side effects. This looks to be a promising step in developing future clinical immune therapies for DIPG.