December 19, 2019
Side Effects of Common Brain Cancer Chemotherapy Medications
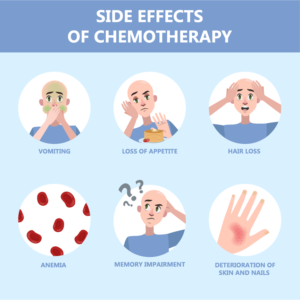
One thing that almost all patients with brain cancer share is experiencing the side effects of the treatment for their tumor. Unwanted or problematic effects of medication that are beyond the intended scope of their use are all side effects. They might be minor, or they could be extremely debilitating, but side effects are usually consistent, and once you’re used to the medication, they can even be fairly predictable. Knowing what to look for can help you and your treatment team manage side effects as they occur.
How chemotherapy drugs work to treat brain cancer
Cytotoxic and cytostatic: Two treatment strategies
All chemotherapy medications are meant to disrupt the way that cancerous cells duplicate, causing tumors to grow, however there are two major categories of chemo drugs. Cytotoxic medications work by killing the cells directly, while cytostatic medications are meant to stop the cells from dividing. It is important to note that any chemotherapy medication will affect both healthy and cancerous cells, a process that may produce a wide array of side effects in patients.
Cytostatic chemotherapy treatments, because they work by preventing cells from dividing, may have especially negative consequences for renewable tissues such as hair and bone marrow.
How common are side effects from medications used to treat brain cancer?
Side effects are extremely common among patients receiving chemotherapy of any kind, in fact one study found that 86% of patients experienced at least one side effect during their chemotherapy treatment. However, while all chemotherapy treatments have common side effects, patients shouldn’t expect to experience all of the common side effects associated with a specific medication. Just like each brain tumor is unique, so is the experience of each patient.
The side effects we’ve listed below are understood to be “common” among patients, meaning that over 30% of people who use the medication report experiencing one or more of the symptoms.
Are side effects for chemotherapy treatment of brain cancer treatable or reversible?
Yes. Your treatment team can help you with additional medications to ease your experience of any side effects that you may be experiencing during chemotherapy. Some people find that keeping a journal to track your medication and any reactions helps to track side effects, making it easier to report any issues to your doctor.
Additionally, almost all side effects are reversible, meaning they should disappear after a chemo treatment cycle is complete. Some may fade quickly, in a few days, while others may take a few weeks to completely resolve.
Avastin (Bevacizumab)
- Generalized Weakness
- Pain
- Abdominal pain
- Nausea & vomiting
- Poor appetite
- Constipation
- Upper respiratory infection
- Low white blood cell count (This can put you at increased risk for infection)
- Proteinuria (kidney problems)
- Nose bleed
- Diarrhea
- Hair loss
- Mouth sores
- Headache
Carboplatin
- Low blood counts (including red blood cells, white blood cells and platelets)
- Nausea and vomiting usually occurring within 24 hours of treatment
- Taste changes
- Hair loss
- Weakness
- Blood test abnormalities: Abnormal magnesium level
Cisplatin
- Nausea and vomiting. Nausea may last up to 1 week after therapy. Anti-nausea medication is given before the infusion, and a prescription is also given for use after.
- Low blood counts. Your white and red blood cells and platelets may temporarily decrease. This can put you at increased risk for infection, anemia, and/or bleeding.
- Kidney toxicity. Effects on kidney function are dose related, observed 10-20 days after therapy, and are generally reversible.
- Ototoxicity hearing loss, ringing in the ears.
- Blood test abnormalities (low magnesium, low calcium, low potassium)
Irinotecan
- Diarrhea; two types early and late forms.
- Early diarrhea: Occurring within 24 hours of receiving drug, accompanied by symptoms runny nose, increased salivation, watery eyes, sweating, flushing, abdominal cramping. (This can occur while the drug is being administered. If so, alert your healthcare professional promptly. Medication can be given to stop and/or lessen this early side effect).
- Late diarrhea: Occurring greater than 24 hours of receiving drug, usually peaks at about 11 days after treatment. Because of concerns of dehydration and electrolyte imbalances with diarrhea it is important to be in contact with health care professionals for monitoring, and for medication and diet modifications advice.
- Nausea and vomiting.
- Weakness.
- Low white blood cell count. (This can put you at increased risk for infection).
- Low red blood cell count (anemia).
- Hair loss
- Poor appetite
- Fever
- Weight loss
Lomustine
- Low blood counts (bone marrow suppression). Your white and red blood cells and platelets may temporarily decrease. This can put you at increased risk for infection, anemia and/or bleeding.
- Nausea and vomiting. Usually within 3-6 hours of taking medication. Taking dose at bedtime, with an anti-nausea medication, significantly reduces the incidence and severity of this side effect.
Temodar (Temozolomide)
- Nausea and vomiting
- Constipation
- Headache
- Fatigue
More Information and Related Sources:
https://www.cancer.gov/about-cancer/treatment/drugs/brain
https://2knaef3o0jpz4ff42k23tr6l-wpengine.netdna-ssl.com/wp-content/uploads/2018/03/chemotherapy.pdf