February 27, 2020
Using ultrasound get powerful drugs into the brain
Recently a new technique that uses ultrasound waves to improve drug penetration into brain tumors has entered clinical testing on human patients, with promising results.
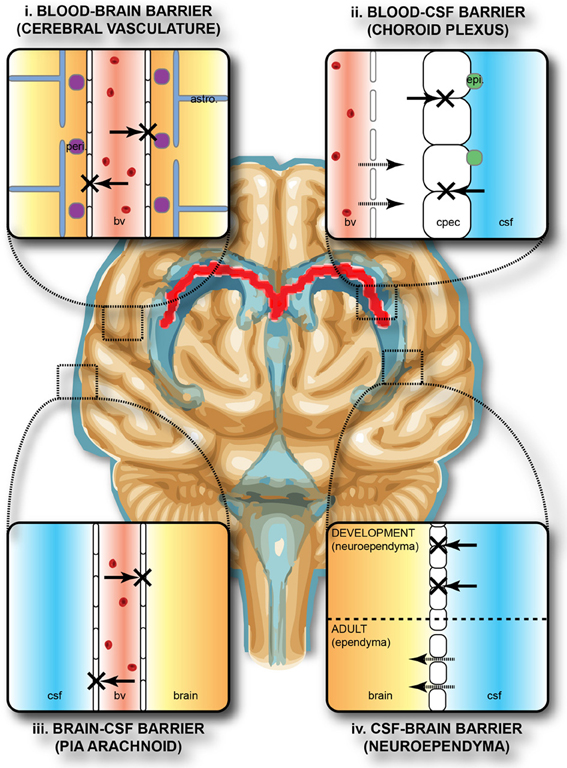
We talk about the blood-brain barrier (BBB) pretty often around here. The BBB, an important structure that keeps healthy brain tissue safe from infections, also blocks most medications from being able to reach their targets in patients with brain tumors.
As a result, scientists have reported concentrations of chemotherapy drugs can be as much as 40 times lower at the center of the tumor compared to the edge. In other words, powerful drugs circulate the bloodstream, where they may cause side effects, but can barely make an impact where they’re needed most.

A number of research teams have identified a strategy for better glioblastoma treatments: rather than focusing on new drugs, they’re interested in ways that the BBB might be bypassed, so that drugs known to be effective in other cancers might also become effective for brain tumors.
Most strategies to overcome the BBB have clear disadvantages. For instance, injecting drugs through the cranium or using pressure gradients on infusion catheters have some of the same safety concerns as surgery. Chemical techniques, such as using insulin receptors to bypass the BBB also work, but it has proven hard to limit the effect just to the tumor region, again raising safety concerns.
An exciting possibility that seems like it will avoid most of these safety downsides is the use of ultrasound waves, which are applied at the same time as chemotherapy infusion.
In one version of this technique, ultrasound from 1024 individually driven transducer elements surrounding the skull under real-time image guidance, is delivered with sub-millimeter accuracy. Through this technique, the BBB is physically disrupted, allowing a wide range of chemotherapy drugs to enter the brain and attack a tumor.
The research team behind one of the major studies in this technique, working out of the Sunnybrook Research Institute in Toronto, Canada, reported their findings after testing the technique on five patients. This initial small study was intended to test feasibility and safety. According to the team, the technique appears “safe, and reversible, and well tolerated among this preliminary group of patients.”
Resources
- Science Daily – Ultrasound blasts potent glioblastoma drug into brain tumor
- Focused Ultrasound Strategies for Brain Tumor Therapy
- Focused ultrasound to open blood-brain barrier could transform glioblastoma treatment delivery
- Nature – Blood-Brain Barrier Opening in Primary Brain Tumors with Non-invasive MR-Guided Focused Ultrasound: A Clinical Safety and Feasibility Study